Phase 1: Focus Groups
To begin, we ran focus groups to get impressions and assessments of traditional presentation formats for diagnostic accuracy. Calculations for these values are traditionally taught using complicated grids such as the one presented to the right.
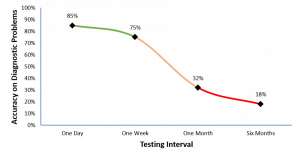
Major takeaway: Not only are patients confused by numbers, but doctors are as well! Lo and behold, doctors hate numbers almost as much as my stat 101 students do. These findings informed a set of longitudinal studies to assessed formal learning of predictive values in a classroom setting.
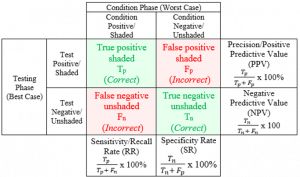
Traditional grid for calculating important diagnostic test result values.





 Solution
Solution